

No-cost or low-cost health coverage from UnitedHealthcare Community Plan. Learn about United Healthcare (NJ FamilyCare) health plans we offer in New Jersey.
All New Jerseyans deserve affordable health care, including you. At UnitedHealthcare Community Plan, we help people live healthier lives. We’ve worked hard to deliver on that mission in New Jersey since 1989.
We offer plans to help New Jerseyans get healthy — and stay healthy. We cover adults, people with disabilities, expecting moms and children with our New Jersey Medicaid and NJ FamilyCare plans. We offer a Dual Special Needs Plans for those who qualify for both New Jersey Medicaid (FamilyCare) and Medicare.
We’re proud that our NJ Medicaid (FamilyCare) plan is accredited by the National Committee for Quality Assurance (NCQA). NCQA is a private, non-profit organization dedicated to improving health care quality. UnitedHealthcare Community Plan of NJ has also achieved NCQA’s Long-Term Services and Supports Distinction for our UnitedHealthcare Dual Complete® plan.


Whatever plan you choose, UnitedHealthcare will help you get the care you need.
It’s easy to enroll. Visit njfamilycare.org or call the NJ FamilyCare phone number at 1-800-701-0710, TTY 1-800-701-0720.
1 Benefits, features, and/or devices vary by plan/area. Limitations, exclusions and/or network restrictions may apply. Other hearing exam providers are available in the UnitedHealthcare network. The plan only covers hearing aids from a UnitedHealthcare Hearing network provider.



As a UnitedHealthcare NJ Medicaid (FamilyCare) member, you’ll get great benefits like:

New Jerseyans on a UnitedHealthcare Dual Special Needs plan (or dual health plan) get many extra benefits beyond those you get with either Original Medicare or Medicaid (FamilyCare).

The Managed Long Term Services and Supports (MLTSS) program is focused on serving frail, elderly and disabled individuals. This program combines traditional health care benefits (doctor visits, hospital stays, labs) and long-term services and supports (providing help in home or community with daily living activities) such as:

$0 copay virtual provider visits to discuss non-emergency medical concerns or general mental health conditions from home.
Speak to network medical or mental health providers using your computer or mobile device. Find participating providers online.

Our program will help you take the right steps to keep you and your baby healthy. We will help you:

You and your providers need to understand each other. Not speaking English makes this difficult. We can arrange for an interpreter to be at your appointments.

Our HealthTalk newsletter is now online. The newsletters are a great way to learn about our health plan and important health topics.
You can read it whenever, wherever you want. Check back quarterly for a new edition.
Medicaid Newsletter English | Español
Senior Newsletter English | Español

Renew Active is the gold standard in Medicare fitness programs for body and mind and can help keep you active at a gym or from home. It’s available with many UnitedHealthcare Dual Complete® plans, at no cost.
You get a free gym membership at a nearby fitness location that you select from our network.* Most members have a location within just a few miles, some with a pool. You can also bring a family member or a friend to the gym with you to assist in your workout at no cost. If you prefer to work out from home, you can view thousands of on-demand digital videos and live streaming fitness classes.
Renew Active includes:
*The Renew Active program varies by plan/area. Access to gym and fitness location network may vary by location and plan.

UnitedHealthcare Community Plan of New Jersey offers free health education workshops to help everyone live healthier lives. We offer programs for children, parents and seniors, and that cover men and women’s health issues.
Workshop topics include:
• Asthma • Lead poisoning • Childhood obesity • Cyber-bullying • Diabetes • Heart disease • Injury prevention • Medication safety • Nutrition • Make your doctor’s visit worthwhile • Parenting skills • Stress management • Understanding breast cancer • Baby showers for expectant moms
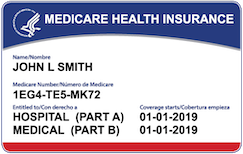
Dual Special Needs Plans (also called dual health plans or D-SNPs for short) are for people who get both Medicaid (FamilyCare) and Medicare. Dual plans cover doctor visits, hospital stays and prescription drugs. They offer more benefits and extras than Original Medicare. You’ll keep all your New Jersey Medicaid (FamilyCare) benefits too.

NJ Medicaid (FamilyCare) is health insurance for people with low incomes. You might be able to get Medicaid (FamilyCare) in New Jersey. if you’re pregnant, have children or live with a disability. In some cases, other adults also may qualify. Costs to you are low and based on your ability to pay. It’s important to know that Medicaid (FamilyCare) rules and coverage differ from state to state.
Disclaimer information (scroll within this box to view)Looking for the federal government’s Medicaid website? Look here at Medicaid.gov.
Plans are insured through UnitedHealthcare Insurance Company or one of its affiliated companies, a Medicare Advantage organization with a Medicare contract and a contract with the State Medicaid Program. Enrollment in the plan depends on the plan’s contract renewal with Medicare. This plan is available to anyone who has both Medical Assistance from the State and Medicare. Benefits, features and/or devices vary by plan/area. Limitations, exclusions and/or network restrictions may apply. Benefits, premiums and/or co-payments/co-insurance may change on January 1 of each year.
Dual Special Needs plans have a $0 premium for members with Extra Help (Low Income Subsidy).
Benefits, features, and/or devices vary by plan/area. Limitations, exclusions and/or network restrictions may apply.
This service should not be used for emergency or urgent care needs. In an emergency, call 911 or go to the nearest emergency room. The information provided through this service is for informational purposes only. The nurses cannot diagnose problems or recommend treatment and are not a substitute for your provider's care. Your health information is kept confidential in accordance with the law. The service is not an insurance program and may be discontinued at any time. Nurse Hotline not for use in emergencies, for informational purposes only.
UnitedHealthcare Connected® for MyCare Ohio (Medicare-Medicaid plan) is a health plan that contracts with both Medicare and Ohio Medicaid to provide benefits of both programs to enrollees.
UnitedHealthcare Connected® (Medicare-Medicaid plan) is a health plan that contracts with both Medicare and Texas Medicaid to provide benefits of both programs to enrollees.
UnitedHealthcare Connected® for One Care (Medicare-Medicaid plan) is a health plan that contracts with both Medicare and MassHealth (Medicaid) to provide benefits of both programs to enrollees.
This is not a complete list. The benefit information is a brief summary, not a complete description of benefits. For more information contact the plan or read the member handbook. Limitations, copays and restrictions may apply. For more information, call UnitedHealthcare Connected® Member Services or read the UnitedHealthcare Connected® member handbook.
UnitedHealthcare Senior Care Options (SCO) is a Coordinated Care plan with a Medicare contract and a contract with the Commonwealth of Massachusetts Medicaid program. Enrollment in the plan depends on the plan’s contract renewal with Medicare. This plan is a voluntary program that is available to anyone 65 and older who qualifies for MassHealth Standard and Original Medicare and does not have any other comprehensive health Insurance, except Medicare. If you have MassHealth Standard, but you do not qualify for Original Medicare, you may still be eligible to enroll in our MassHealth Senior Care Option plan and receive all of your MassHealth benefits through our Senior Care Options (SCO) program.
Every year, Medicare evaluates plans based on a 5-Star rating system. The 5-Star rating applies to plan year 2024.
The choice is yours
We will provide you with information to help you make informed choices, such as physicians' and health care professionals' credentials. This information, however, is not an endorsement of a particular physician or health care professional's suitability for your needs.
The providers available through this application may not necessarily reflect the full extent of UnitedHealthcare's network of contracted providers. There may be providers or certain specialties that are not included in this application that are part of our network. If you don't find the provider you are searching for, you may contact the provider directly to verify participation status with UnitedHealthcare's network, or contact Customer Care at the toll-free number shown on your UnitedHealthcare ID card. We also recommend that, prior to seeing any physician, including any specialists, you call the physician's office to verify their participation status and availability.
Some network providers may have been added or removed from our network after this directory was updated. We do not guarantee that each provider is still accepting new members.
Out-of-network/non-contracted providers are under no obligation to treat UnitedHealthcare plan members, except in emergency situations. Please call our customer service number or see your Evidence of Coverage for more information, including the cost- sharing that applies to out-of-network services.
In accordance with the requirements of the federal Americans with Disabilities Act of 1990 and Section 504 of the Rehabilitation Act of 1973 ("ADA"), UnitedHealthcare Insurance Company provides full and equal access to covered services and does not discriminate against qualified individuals with disabilities on the basis of disability in its services, programs, or activities.
Network providers help you and your covered family members get the care needed. Access to specialists may be coordinated by your primary care physician.
Paper copies of the network provider directory are available at no cost to members by calling the customer service number on the back of your ID card. Non-members may download and print search results from the online directory.
To report incorrect information, email provider_directory_invalid_issues@uhc.com. This email box is for members to report potential inaccuracies for demographic (address, phone, etc.) information in the online or paper directories. Reporting issues via this mail box will result in an outreach to the provider’s office to verify all directory demographic data, which can take approximately 30 days. Individuals can also report potential inaccuracies via phone. UnitedHealthcare Members should call the number on the back of their ID card, and non-UnitedHealthcare members can call 1-888-638-6613 / TTY 711, or use your preferred relay service.
If you’re affected by a disaster or emergency declaration by the President or a governor, or an announcement of a public health emergency by the Secretary of Health and Human Services, there is certain additional support available to you.
If CMS hasn’t provided an end date for the disaster or emergency, plans will resume normal operation 30 days after the initial declaration.