Roderick J Finlayson MD FRCPC
Associate Professor Department of Anesthesia, McGill University,
Medical director, Chronic Pain Program,
McGill University Health Center, Montreal, Canada
Section Editor: David Provenzano, MD
Cervical medial branch blocks (CMBBs) and third occipital nerve blocks (TONBs) are commonly used in the diagnosis and treatment of chronic neck pain and headaches.
Although fluoroscopy constitutes the imaging standard for CMBB and TONB, ultrasonography (US) is particularly well-suited for these procedures as the articular pillars (APs) are situated well within the visual range of high frequency probes. Moreover, unlike fluoroscopy, US may enable the operator to identify (and circumvent) critical soft tissue structures such as blood vessels.
Although the larger third occipital nerve can be visualized with US in most patients, the smaller medial branches at other levels are often difficult to identify in clinical practice. Therefore, the landmark-based technique described below does not rely solely on neural identification, but instead targets a point on the bony contour of the cervical spine corresponding to the centroid of the AP. A posterolateral in-plane approach is used, with placement of the needle tip between the periosteum and the semispinalis capitis muscle, allowing small volumes of injectate to cover the lateral surface of the AP and block the medial branch.
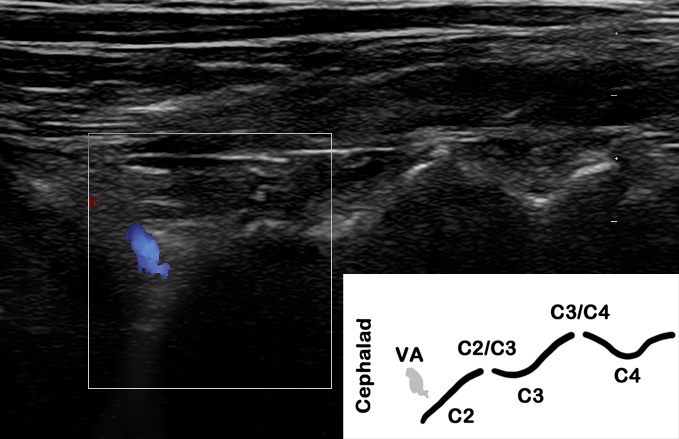
Figure 1: Coronal scan of the upper cervical spine along the anterior edge of the articular pillars with color power doppler mode engaged. The drop off at the C2/C3 level is confirmed by imaging the vertebral artery cephalad. Vertebral artery (VA); inferior articular process of C2 (C2); articular pillars (C3, C4); zygapophyseal joints (C2/C3, C3/C4)
Coronal (long axis) scan. This view is used for level confirmation in both the upper and lower cervical spines. In the long axis, the APs appear as a series of peaks (zygapophyseal joints lines) and valleys (convex shapes of the APs). Above the C2-C3 joint, the slope of the inferior articular process of C2 creates a characteristic drop off with the vertebral artery visible immediately cephalad to it (Fig 1). In the lower cervical spine, the transverse process (TP) of C7, which can be found anterior to the AP, provides a reference for needle positioning. The medial branches can often be imaged in the coronal plane as they cross the APs, in close proximity to the periosteal contour. [ 1]
Transverse (short axis) scan. This view is used for needle placement. The targets are the C2-C3 zygapophyseal joint (TON) and the centroid aspect of the AP (C3-C6 medial branches). The latter appears as a distinctive flat hyperechoic line that can be appreciated when moving the probe in a cephalo-caudal direction . It can be easily differentiated from the joint line, which is rounded and less echogenic. The tendinous insertions of the semispinalis capitis muscle (SSC) can be identified just above the AP; their importance lies in the fact that they restrict the injectate to the periosteal plane, thus ensuring a successful block with small volumes of local anesthetic (LA; Fig 2). A useful landmark in the lower cervical spine is the narrow TP of C7, which has no anterior tubercle: this permits its differentiation from the TPs of other cervical levels and the wider square shape of the T1 TP .
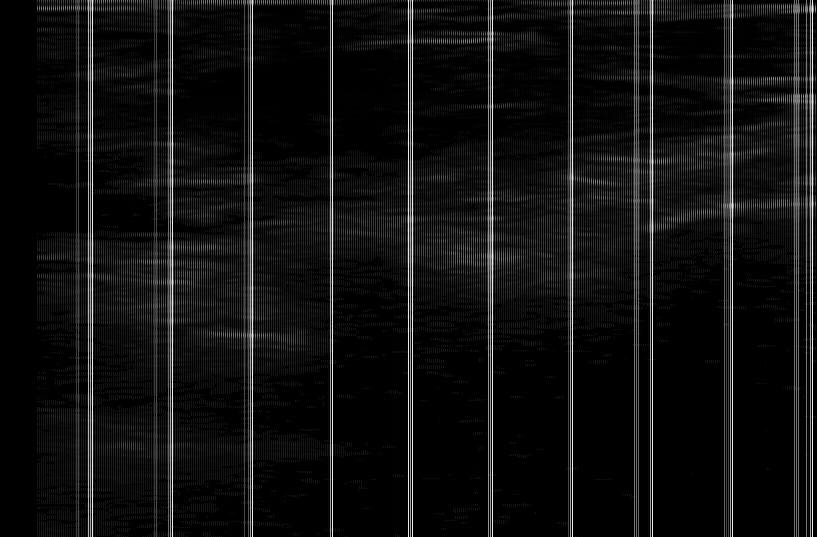
Figure 2: Transverse scan of the C4 articular pillar (AP) showing a needle in position after injection of 0.3 mL of local anesthetic. The injectate has spread along the anteroposterior aspect of the AP, lifting up the semispinalis capitis muscle (SSC). Posterior tubercle of transverse process (PT); needle (N); lamina (Lam)
Patients are placed in the lateral decubitus position with the head supported in a neutral position. An L14-5 MHz linear array probe and a 2.5 inch, 22- or 25-gauge block needle are commonly employed. I have found that a reduction in the dynamic range (increase in the image contrast) facilitates visualization of the targets on the APs.
TON, C3, C4 medial branch. The neck is first scanned in the coronal plane along the posterior edge of the AP in order to identify the drop-off at the C2-C3 level. Further confirmation is sought by imaging the vertebral artery (cephalad and anterior). The probe is then rotated to a transverse plane, and the C2-C3 zygapophyseal joint identified, for the third occipital nerve block. From this point, the probe is moved caudally to the target points on the C3 and C4 APs.
C5, C6 medial branch. The base of the neck is scanned in the transverse plane and the TP of T1 identified. As the probe is moved cephalad from this point, the TP of C7 is localized, followed by the targets on the AP of C6 and C5. The superior articular process of C7 can be occasionally imaged cephalad to the TP of C7: if prominent, it could be mistaken for the C6 AP .
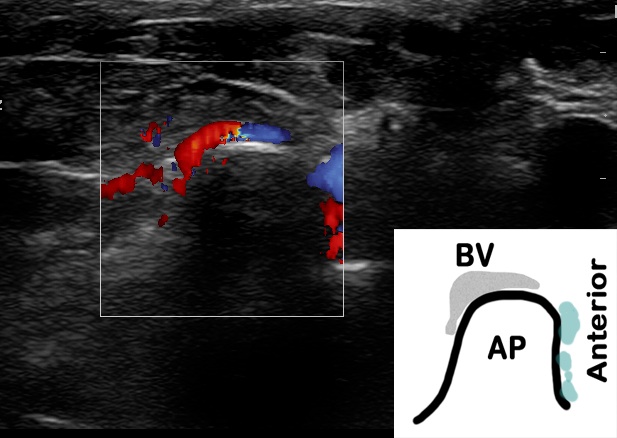
Figure 3: Transverse scan of the C5 articular pillar (AP) with color power doppler mode engaged. The blood vessel was identified prior to needle insertion and successfully avoided
Needle placement after target level has been identified. Once the target has been identified in the transverse plane, pressure on the probe is reduced and the color doppler mode engaged to detect potential blood vessels in the needle path (Fig 3). A posterolateral in-plane approach is used. The needle is advanced until contact with the periosteum. The probe is then rotated to obtain a coronal scan, and the needle confirmed to be in the middle of the targeted AP. Returning to a transverse view, LA is then injected under real time visualization; if necessary, the position of the needle tip is adjusted to obtain a sub-SSC LA spread that covers the anteroposterior diameter of the AP or joint for TONB (Figs. 4a & 4b ). The extent of cephalocaudal spread can be documented in the coronal plane. When performing a TONB, needle placement can be further refined by placing the tip next to the nerve as it can often be imaged near the C2-C3 joint in the coronal plane.
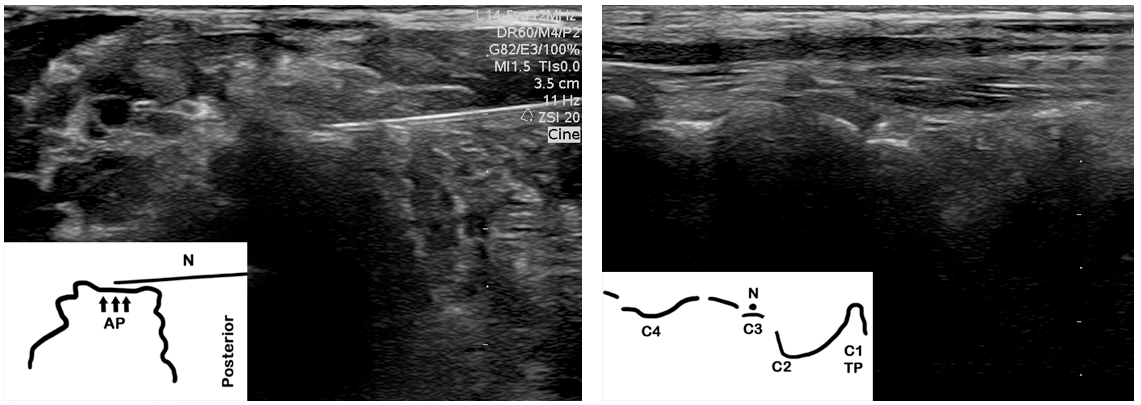
Figure 4: Images documenting successful needle placement for a C3 medial branch block in a 73 years old patient with degenerative changes altering the bony contours of the articular pillars (AP). Figure 4a: transverse scan of the C3 AP demonstrating a needle (N) in position on the sonographic target representing the centroid of the AP (arrows). Figure 4b: coronal scan of the upper cervical spine confirming appropriate needle positioning. The APs of C3 and C4 can be seen, however the contours of the zygapophyseal joints have been distorted by osteophytes. Inferior articular process of C2 (C2); C1 transverse process (C1 TP).
Major complications are rare after CMBBs. However, in a recent study examining 7482 fluoroscopy-guided facet nerve blocks, [ 2] adverse events such as vascular breach and hematoma were found to occur most frequently at the cervical level, with incidences of 20% and 2.3% respectively. Ultrasonography provides a two-dimensional view of the AP, as well as real time visualization of the needle tip as it advances towards the target. In turn, this may allow the operator to avoid blood vessels and other critical structures. In contrast, fluoroscopy provides only intermittent visualization and relies on small interrupted needle movements with the maintenance of a true lateral view to avoid misdirection. In addition, the posterolateral approach (US) may offer additional safety advantages in comparison to the lateral fluoroscopy approach since critical structures are shielded by the APs and TPs. Further studies are required to confirm these theoretical advantages and determine the level of experience required to safely perform US guided CMBBs.
In a 2-part study involving 53 patients and 209 CMBBs, [ 3] we first examined the ability of US to provide accurate needle placement on the AP using an in-plane approach. Fluoroscopic control demonstrated that the needles were adequately positioned in the middle 2 quarters of the AP 80.1% of the time; in the remaining 19.9% of cases, they were positioned in the outer quarter. In the second phase, 0.3 mL of a LA-iodinated contrast mixture was injected under US using a posterolateral approach and the spread verified on anteroposterior and lateral X-ray views. Our results showed that accuracy varied by level: TON (100%), C3 (100%), C4 (97.7%), C5 (91.4%), C6 (84.9%). Contrast spread leading to complete coverage of an adjacent non-targeted level was seen in 13.5% of blocks. Since the completion of this study, we have observed that the additional step of confirming the level in the coronal plane increases accuracy at the C5 and C6 levels . In a recent randomized trial (n = 40), 4 we compared US and fluoroscopy for TONB and found similar success rates, contrast distribution and sensory block. However, the performance time and number of needle passes were significantly decreased with US. In both of our studies, no complications were noted. Blood vessels overlying the target were recorded on US scan in 8 % to 10% of blocks. Because of the variable position of the C7 medial branch, the recommended fluoroscopic approach involves multiple injections; [ 5] to date, an equivalent US technique has yet to be validated.